purple plum aesthetics blog
The Link Between Oral Health and Systemic Conditions

Modern research reveals that oral health’s inextricable connection with systemic health extends beyond the mouth. Poor oral health contributes to chronic inflammation that affects the heart, lungs, and metabolism. Patients who focus on complete wellness through holistic preventative dentistry in Falls Church, Virginia, US can help protect not only their teeth and gums but also their long-term general health.
Understanding Oral and Systemic Health
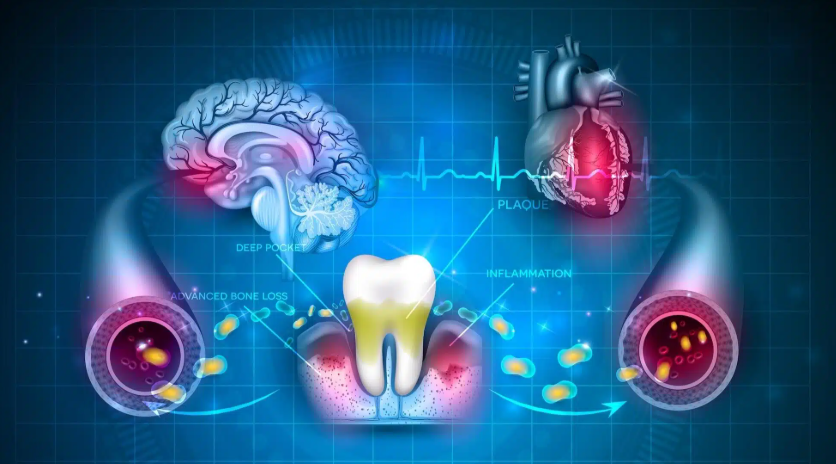
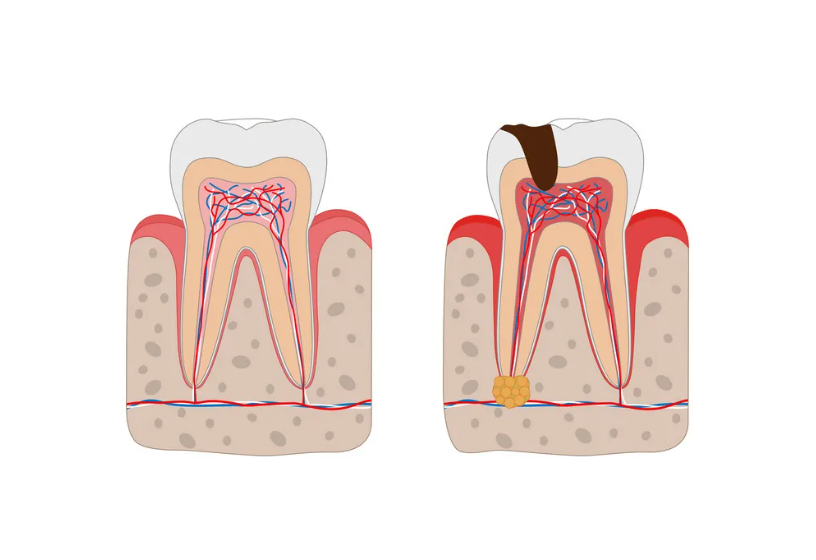
The relationship between oral and systemic health is now a central focus of both dental and medical professionals. Periodontal disease remains one of the most widespread chronic diseases, and its effects go far beyond tooth loss. Bacteria from gum infections enter the bloodstream, triggering systemic inflammation that contributes to cardiovascular disease, diabetes mellitus, and respiratory illnesses.
Oral health professionals view the oral cavity as a key reflection of overall wellness. When chronic inflammation or infection persists, it can influence systemic conditions and worsen outcomes for patients already managing long-term health issues.
How Periodontal Disease Affects Systemic Health
Bacterial Spread and Oral Focal Infection
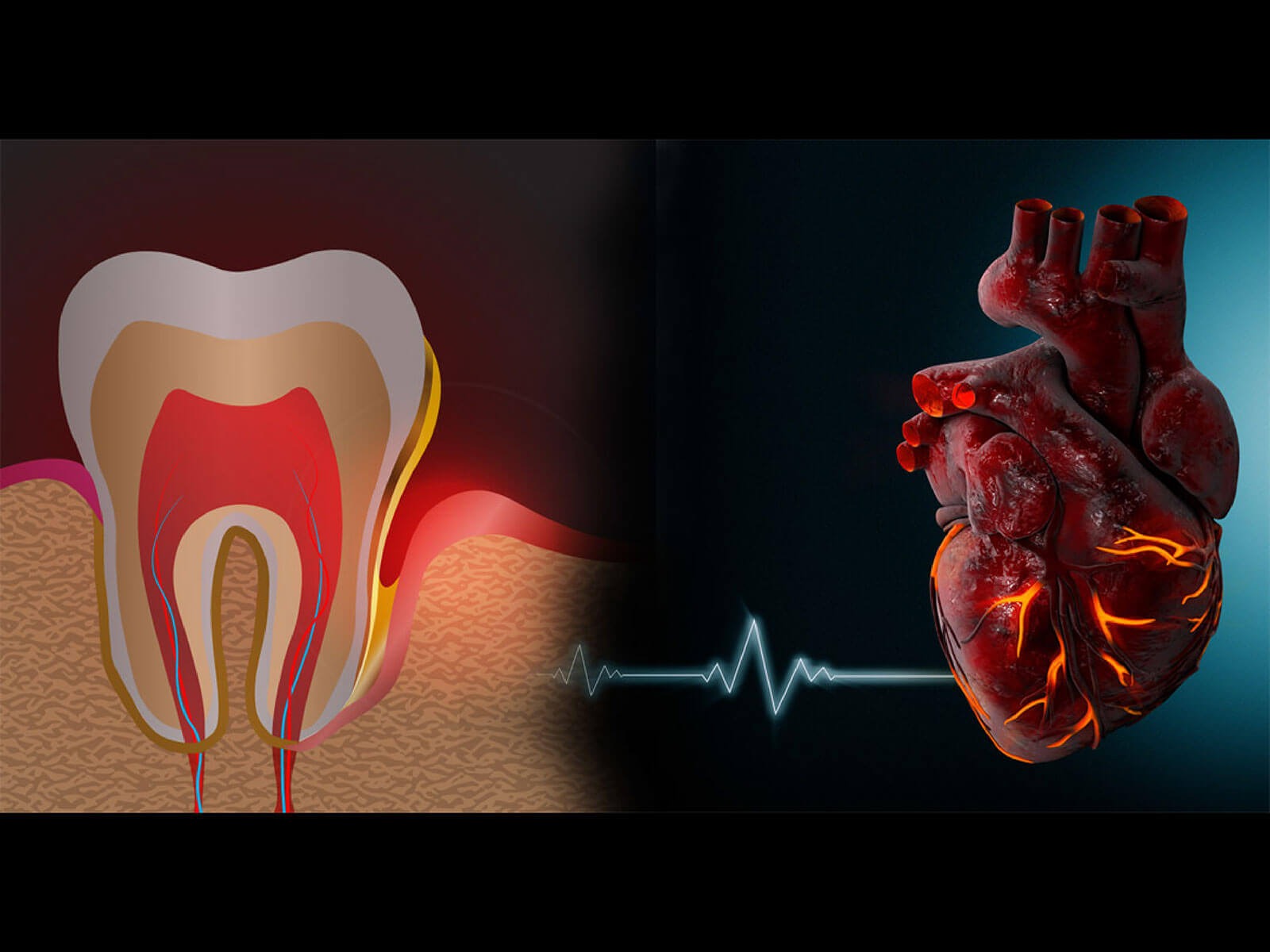
The concept of the oral focal infection theory explains how oral bacteria can travel through blood vessels and reach distant organs. Periodontal pathogens such as Porphyromonas gingivalis have been identified in arterial plaque, suggesting a role in atherosclerotic cardiovascular disease and coronary heart disease.
Systemic Inflammation and Immune Response
Periodontal infection triggers immune activity that releases inflammatory molecules such as tumor necrosis factor alpha and interleukin-6. These chemicals contribute to chronic systemic inflammation, a key factor connecting periodontal disease with other chronic diseases. Prolonged inflammation damages tissues and organs throughout the body.
Shared Risk Factors and Common Pathways
Poor diet, tobacco use, and inadequate oral hygiene are common risk factors for both oral and systemic conditions. These habits alter the oral microbiome, increase chronic inflammation, and compromise immune defense, creating an ideal environment for both dental diseases and systemic disorders to thrive.
Oral Health and Cardiovascular Disease
Studies show a clear link between periodontal disease and cardiovascular health. Oral bacteria from infected gums can adhere to damaged arteries, encouraging plaque buildup. Chronic inflammation from severe periodontitis contributes to endothelial dysfunction, which raises the risk of heart disease and stroke. Maintaining periodontal health and pursuing regular periodontal treatment help lower systemic inflammation and support healthy blood flow.
Oral Health and Diabetes Mellitus
People with diabetes face a higher likelihood of developing periodontal infection, while gum inflammation can make glycemic control more difficult. This two-way relationship increases systemic complications. Professional periodontal therapy has been shown to improve blood sugar stability by reducing bacterial load and systemic inflammation. Integrating dental care with diabetes management helps patients achieve better disease control and overall systemic health.
Oral Health and Respiratory Diseases
Respiratory diseases often stem from bacterial aspiration from the oral cavity into the lungs. Chronic periodontitis and poor oral hygiene increase the risk of infections such as pneumonia and bronchitis. Older adults and patients with weakened immunity are especially vulnerable. Maintaining oral health and controlling dental plaque are vital steps to prevent respiratory complications.
Oral Health and Pregnancy Outcomes
Emerging evidence suggests that gum disease can affect pregnancy outcomes. Inflammatory mediators from periodontal infections may contribute to preterm birth and low birth weight. Periodontal therapy during pregnancy supports healthier outcomes for both mother and baby, making early diagnosis and preventive care critical.
Oral Health and Neurological Conditions
Research into dental and craniofacial health shows that chronic periodontal infection may contribute to Alzheimer’s disease. Oral bacteria and inflammation have been detected in brain tissue, suggesting a possible connection between oral infection and cognitive decline. Maintaining oral hygiene and seeking early treatment for gum disease may reduce this risk.
Oral Health and Rheumatoid Arthritis
Rheumatoid arthritis and periodontitis share similar immune responses and chronic inflammation patterns. Periodontal pathogens can trigger an immune reaction that mimics those seen in joint inflammation. Treating gum disease can lower systemic inflammation and help patients manage arthritis more effectively.
Prevention and Oral Health Behaviors
Maintaining oral health is central to preventing systemic diseases. Effective oral hygiene practices, balanced nutrition, and regular dental visits reduce inflammation and bacterial growth. Avoiding tobacco and nicotine products protects gums and supports overall wellness. Dental professionals emphasize the importance of early diagnosis and coordinated care between dental and medical providers.
Public health awareness programs promoting good oral hygiene and disease prevention strategies can improve outcomes across populations. Early detection of oral health issues benefits systemic health outcomes and reduces healthcare burdens.

Conclusion
Oral health and systemic health are deeply connected. Chronic inflammation and oral bacteria can affect blood vessels, organs, and immune responses throughout the body. Maintaining good oral hygiene, receiving timely periodontal treatment, and working closely with dental and medical professionals help prevent chronic diseases like cardiovascular disease, diabetes mellitus, respiratory disorders, rheumatoid arthritis, and adverse pregnancy outcomes.
By prioritizing holistic dental care and consistent oral health behaviors, patients strengthen both their smiles and their overall well-being. Taking proactive steps through professional dental care supports healthier systemic conditions and a better quality of life for years to come.
Benefits of Periodontal Therapy
Periodontal therapy offers several significant benefits that extend beyond just oral health. Here are four key benefits:
One of the primary benefits of periodontal therapy is the prevention of tooth loss. Periodontal disease, if left untreated, can lead to the destruction of the bone and connective tissue that support the teeth.
Periodontal disease is associated with chronic inflammation, which can have adverse effects on overall health. By treating periodontal disease, patients can reduce systemic inflammation, potentially lowering the risk of related health conditions such as cardiovascular disease, diabetes, and rheumatoid arthritis.
Periodontal therapy helps improve oral hygiene by thoroughly cleaning the pockets around the teeth, which are difficult to clean with regular brushing and flossing alone.
Healthier gums appear firm and pink, which contributes to an overall more attractive smile. Additionally, periodontal treatment can stabilize teeth and prevent further recession, helping patients maintain a youthful and confident appearance.

